Coronary artery disease and coronary artery bypass grafting(CABG)
動脈硬化是隨著年齡的增長,全身性的慢性血管壁粥狀病變,而冠狀動脈粥狀硬化也受遺傳及環境因素的影響,如高膽固醇血症(hypercholesterolemia),糖尿病(diabetes mellitus),高血壓(hypertension),抽煙(smoking),老化(aging),肥胖(obesity)生活型態(life style),家族遺傳(family history)…,冠狀動脈血管的硬化狹窄及粥狀物破裂阻塞血管是造成突發且毫無預警的急性心肌梗塞的主因。冠狀動脈的功能是在供應心肌細胞血流,提供心肌本身所需的氧氣及養分。當冠狀動脈發生阻塞時,因心肌缺血,所以病患會有心絞痛的情形發生,大多為胸悶或胸痛,嚴重時會導致心臟衰竭、心肌梗塞及死亡!目前大部份的冠狀動脈狹窄都可以用冠狀動脈氣球擴張術(PCI)及冠狀動脈支架(stenting)來治療、輔助。不過,在某些病人及實際情況下,使用冠狀動脈繞道手術會有更佳的效果。傳統的冠狀動脈繞道手術是以體外循環(即人工心肺機)在手術時取代心肺的功能,先使心臟停止跳動,將心臟及大部分血液輸送至心肺機,取代原先心臟及肺臟的功能,以便維持身體所有器官的血流及氧合代謝,再利用大隱靜脈、內乳動脈、橈動脈或胃網膜動脈當作繞道血管的材料,由主動脈出發,跨過狹窄阻塞的冠狀動脈段到後方以避開塞住的區段,以增加心肌血流的供應;而原來狹窄阻塞的部分,則不特別作處置。手術的主要目的,是為了增加心肌血流供應,使心臟功能得以繼續維持,成功率將近95%。目前已發展出不需經人工心肺機進行體外循環的冠狀動脈繞道手術,就是所謂的『心臟不停跳』冠狀動脈繞道手術(beating heart surgery, off-pump coronary artery bypass grafting),此種手術方式是用特殊的穩定器固定需接合血管的部位,使手術部位局部停止跳動,而心臟的其餘部位仍繼續跳動,以維持身體器官的血流供應,可以減少以往使用人工心肺循環機所可能帶來的併發症,如免疫反應、中風、血液稀釋…等,對尿毒症患者術後易出血,免疫下降等不利的影響,並且減少原本心臟功能不佳的病患在經過心肺循環機後常造成心臟無法負荷的傷害。然而,在手術過程中,某些病患可能還是需要使用到人工心肺機;所以都會有一位受過人工心肺機專業訓練的體外循環師隨時待命。另外尚有微創手術(Minimally Invasive Surgery),顧名思義就是透過較小的傷口來完成冠狀動脈繞道手術。由於繞道手術並不能改變基礎代謝情況,所以術後繼續控制危險因子顯得相當重要,要提醒病患記得戒菸、適度運動、減肥、少脂、控制血壓及血糖,以降低冠狀動脈再發生粥狀硬化的病變而再度狹窄。
- Indication for CABG (AHA)
9.2.1. Asymptomatic or Mild Angina (無症狀或輕度心絞痛患者)
Class I
- 左主冠狀動脈狹窄(證據等級:A)
- 左主等效 (Left main equivalant):顯著(大於或等於70%)近端LAD和近端左迴旋動脈狹窄。(證據等級:A)
- 有3-血管疾病的患者可能有用。(在異常LV功能的患者中,存活率的好處更大。) (證據等級:C)
Class IIa
有近端LAD狹窄且有1-或2-血管疾病(如果通過非侵入性研究證明有大量缺血並且/或LVEF小於0.50,則此推薦變為Class I。) (證據等級:A)
Class IIb
考慮在1-或2-血管疾病但未涉及近端LAD的患者中進行CABG(如果在非侵入性測試上滿足大區域的生存心肌和高風險標準,則此推薦變為Class I)。(證據等級:B)
9.2.2. Stable Angina
Class I
1. CABG is recommended for patients with stable angina who have significant left main coronary artery stenosis. (Level of Evidence: A)
2. CABG is recommended for patients with stable angina who have left main equivalent: Significant (greater than or equal to 70%) stenosis of the proximal LAD and proximal left circumflex artery. (Level of Evidence: A)
3. CABG is recommended for patients with stable angina who have 3-vessel disease. (Survival benefit is greater when LVEF is less than 0.50.) (Level of Evidence: A)
4. CABG is recommended in patients with stable angina who have 2-vessel disease with significant proximal LAD stenosis and either EF less than 0.50 or demonstrable ischemia on noninvasive testing. (Level of Evidence: A)
5. CABG is beneficial for patients with stable angina who have 1- or 2-vessel CAD without significant proximal LAD stenosis but with a large area of viable myocardium and high-risk criteria on noninvasive testing. (Level of Evidence: B)
6. CABG is beneficial for patients with stable angina who have developed disabling angina despite maximal noninvasive therapy, when surgery can be performed with acceptable risk. If angina is not typical, objective evidence of ischemia should be obtained. (Level of Evidence: B)
Class IIa
1. CABG is reasonable in patients with stable angina who have proximal LAD stenosis with 1-vessel disease. (This recommendation becomes Class I if extensive ischemia is documented by noninvasive study and/or LVEF is less than 0.50). (Level of Evidence: A)
2. CABG may be useful for patients with stable angina who have 1- or 2-vessel CAD without significant proximal LAD stenosis but who have a moderate area of viable myocardium and demonstrable ischemia on noninvasive testing. (Level of Evidence: B)
Class III
1. CABG is not recommended for patients with stable angina who have 1- or 2-vessel disease not involving significant proximal LAD stenosis, patients who have mild symptoms that are unlikely due to myocardial ischemia, or patients who have not received an adequate trial of medical therapy and
a. have only a small area of viable myocardium or (Level of Evidence: B)
b. have no demonstrable ischemia on noninvasive testing. (Level of Evidence: B)
2. CABG is not recommended for patients with stable angina who have borderline coronary stenoses (50% to 60% diameter in locations other than the left main coronary artery) and no demonstrable ischemia on noninvasive testing. (Level of Evidence: B)
3. CABG is not recommended for patients with stable angina who have insignificant coronary stenosis (less than 50% diameter reduction). (Level of Evidence: B)
9.2.3. Unstable Angina/NSTEMI
Class I
1. CABG should be performed for patients with unstable angina/NSTEMI with significant left main coronary artery stenosis. (Level of Evidence: A)
2. CABG should be performed for patients with unstable angina/NSTEMI who have left main equivalent: significant (greater than or equal to 70%) stenosis of the proximal LAD and proximal left circumflex artery. (Level of Evidence: A)
3. CABG is recommended for unstable angina/NSTEMI in patients in whom revascularization is not optimal or possible, and who have ongoing ischemia not responsive to maximal nonsurgical therapy. (Level of Evidence: B)
Class IIa
CABG is probably indicated for patients with unstable angina/NSTEMI who have proximal LAD stenosis with 1- or 2-vessel disease. (Level of Evidence: A)
Class IIb
CABG may be considered in patients with unstable angina/NSTEMI who have 1- or 2-vessel disease not involving the proximal LAD when percutaneous revascularization is not optimal or possible. (If there is a large area of viable myocardium and high-risk criteria are met on noninvasive testing, this recommendation becomes Class I.) (Level of Evidence: B)
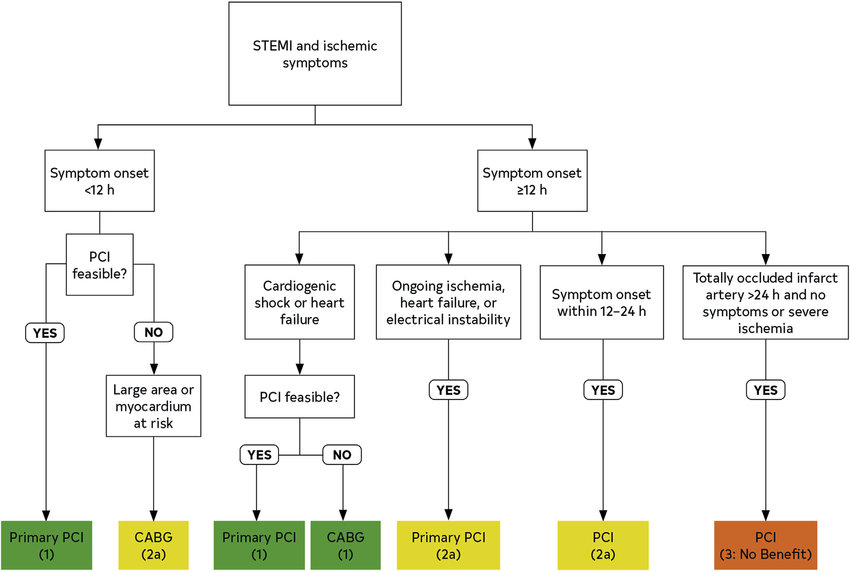
9.2.4. STEMI
Class I
Indications for CABG in ST-Segment Elevation (QWave) MI: None.
Emergency or urgent CABG in patients with STEMI should be undertaken in the following circumstances:
a. Failed angioplasty with persistent pain or hemodynamic instability in patients with coronary anatomy suitable for surgery. (Level of Evidence: B)
b. Persistent or recurrent ischemia refractory to medical therapy in patients who have coronary anatomy suitable for surgery, who have a significant area of myocardium at risk, and who are not candidates for PCI. (Level of Evidence: B)
c. At the time of surgical repair of postinfarction ventricular septal rupture or mitral valve insufficiency. (Level of Evidence: B)
d. Cardiogenic shock in patients less than 75 years old with ST-segment elevation or left bundle-branch block or posterior MI who develop shock within 36 hours of MI and are suitable for revascularization that can be performed within 18 hours of shock, unless further support is futile because of patient’s wishes or contraindications/unsuitability for further invasive care (Level of Evidence: A)
e. Life-threatening ventricular arrhythmias in the presence of greater than or equal to 50% left main stenosis and/or triple-vessel disease (Level of Evidence: B)
Class IIa
1.CABG may be performed as primary reperfusion in patients who have suitable anatomy and who are not candidates for or who have had failed fibrinolysis/ PCI and who are in the early hours (6 to 12 hours) of evolving STEMI. (Level of Evidence: B)
2.In patients who have had an STEMI or NSTEMI, CABG mortality is elevated for the first 3 to 7 days after infarction, and the benefit of revascularization must be balanced against this increased risk. Beyond 7 days after infarction, the criteria for revascularization described in previous sections are applicable. (Level of Evidence: B)
Class III
1.Emergency CABG should not be performed in patients with persistent angina and a small area of myocardium at risk who are hemodynamically stable. (Level of Evidence: C)
2.Emergency CABG should not be performed in patients with successful epicardial reperfusion but unsuccessful microvascular reperfusion. (Level of Evidence: C)
9.2.5. Poor LV Function
Class I
1. CABG should be performed in patients with poor LV function who have significant left main coronary artery stenosis. (Level of Evidence: B)
2. CABG should be performed in patients with poor LV function who have left main equivalent: significant (greater than or equal to 70%) stenosis of the proximal LAD and proximal left circumflex artery. (Level of Evidence: B)
3. CABG should be performed in patients with poor LV function who have proximal LAD stenosis with 2- or 3-vessel disease. (Level of Evidence: B)
Class IIa
CABG may be performed in patients with poor LV function with significant viable noncontracting, revascularizable myocardium and without any of the above anatomic patterns. (Level of Evidence: B)
Class III
CABG should not be performed in patients with poor LV function without evidence of intermittent ischemia and without evidence of significant revascularizable viable myocardium. (Level of Evidence: B)
9.2.6. Life-Threatening Ventricular Arrhythmias
Class I
1. CABG should be performed in patients with life-threatening ventricular arrhythmias caused by left main coronary artery stenosis. (Level of Evidence: B)
2. CABG should be performed in patients with life-threatening ventricular arrhythmias caused by 3-vessel coronary disease. (Level of Evidence: B)
Class IIa
1. CABG is reasonable in bypassable 1- or 2-vessel disease causing life-threatening ventricular arrhythmias. (This becomes a Class I recommendation if the arrhythmia is resuscitated sudden cardiac death or sustained ventricular tachycardia.) (Level of
Evidence: B)
2. CABG is reasonable in life-threatening ventricular arrhythmias caused by proximal LAD disease with 1- or 2-vessel disease. (This becomes a Class I recommendation if the arrhythmia is resuscitated sudden cardiac death or sustained ventricular tachycardia). (Level of Evidence: B)
Class III
CABG is not recommended in ventricular tachycardia with scar and no evidence of ischemia. (Level of Evidence: B)
9.2.7. CABG After Failed PTCA
Class I
1. CABG should be performed after failed PTCA in the presence of ongoing ischemia or threatened occlusion with significant myocardium at risk. (Level of Evidence: B)
2. CABG should be performed after failed PTCA for hemodynamic compromise. (Level of Evidence: B)
Class IIa
1. It is reasonable to perform CABG after failed PTCA for a foreign body in crucial anatomic position. (Level of Evidence: C)
2. CABG can be beneficial after failed PTCA for hemodynamic compromise in patients with impairment of the coagulation system and without previous sternotomy. (Level of Evidence: C)
Class IIb
CABG can be considered after failed PTCA for hemodynamic compromise in patients with impairment of the coagulation system and with previous sternotomy. (Level of Evidence: C)
Class III
1. CABG is not recommended after failed PTCA in the absence of ischemia. (Level of Evidence: C)
2. CABG is not recommended after failed PTCA with inability to revascularize due to target anatomy or no-reflow state. (Level of Evidence: C)
9.2.8. Patients With Previous CABG
Class I
1. Coronary bypass should be performed in patients with prior CABG for disabling angina despite optimal nonsurgical therapy. (If angina is not typical, then objective evidence of ischemia should be
obtained.) (Level of Evidence: B)
2. Coronary bypass should be performed in patients with prior CABG without patent bypass grafts but with Class I indications for surgery for native-vessel CAD (significant left main coronary stenosis, left main equivalent, 3-vessel disease). (Level of Evidence: B)
Class IIa
1. Coronary bypass is reasonable in patients with prior CABG and bypassable distal vessel(s) with a large area of threatened myocardium by noninvasive studies. (Level of Evidence: B)
2. Coronary bypass is reasonable in patients who have prior CABG if atherosclerotic vein grafts with stenoses greater than 50% supplying the LAD coronary artery or large areas of myocardium are present. (Level of Evidence: B)
- 術前評估(Pre-OP Evaluation)
- LV function –LVEF(cardiac sonography, MUGA, LV angiography…)
- Lung function
- Renal function
- PAD(peripheral artery disease) – if there is any PAOD history
- Carotid Sonography – if there is any risk for CVA
- CT scan – check if the aorta is calcified, not suitable for cross clamping
- Coronary angiography – make sure that how many grafts we will
anastomosis for revascularization
- Conduits for revascularizations
- arterial graft
internal thoracic artery, radial artery, right gastroepiploeic artery…
- venous graft
greater saphenous vein graft, cephalic vein graft...
- High Risk for Operation
- Poor LV function
- Previous cardiac operation
- Emergent operation
- Old age
- Female (gender)
- poor renal function